The Clinic: Patrick Ranney & Answers To The 4 Most Common Questions About Herniated Discs
The Clinic: Patrick Ranney & Answers To The 4 Most Common Questions About Herniated Discs https://bestpracticehealth.com/wp-content/uploads/2022/01/My-Post-copy-1-1024x576.jpg 1024 576 Best Practice Health Best Practice Health https://bestpracticehealth.com/wp-content/uploads/2022/01/My-Post-copy-1-1024x576.jpgPatrick Ranney appeared in Episode 2 of The Clinic with Dr. Dan Lieberman complaining of low back pain running like electricity down his left leg. Pat is well known to The Clinic, having undergone L5/S1 anterior lumbar interbody fusion surgery six years earlier. He reports that he was pain free until three weeks earlier.
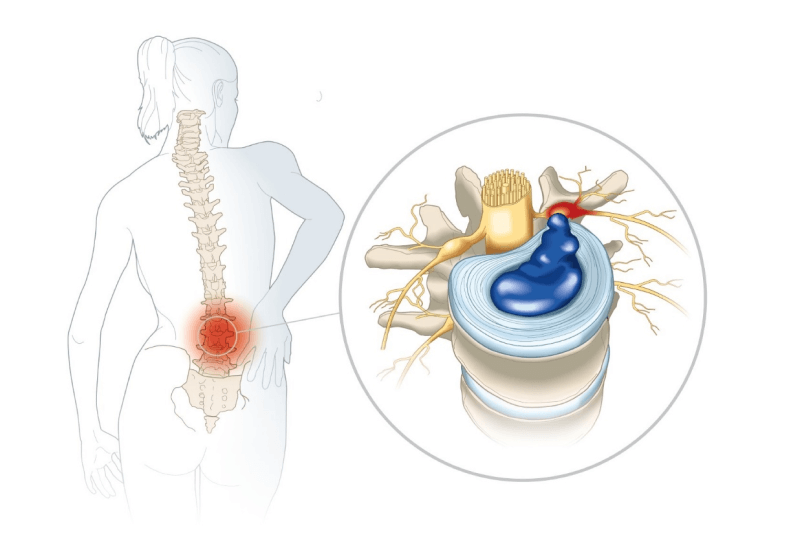
Pat returned to walking for exercise after a couple of months break due to a knee issue. After the second day he reported pain and numbness in his right leg. On physical examination Pat had weakness lifting his left leg straight up. Magnetic resonance imaging (MRI) showed a giant herniated disc in the lumbar spine.
If you just found out, like Pat, that you have a herniated disc or sciatica, I am sorry. The pain is usually severe. Face with that much pain most people tend to panic; and who can blame them. This blog will give you the information you need to make good decisions about your health in dealing with this problem. Your most frequent questions are answered below. 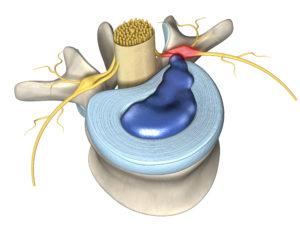
Can a herniated disc heal itself?
Herniated discs normally heal by themselves, but the process is slow and sometimes it is either too painful or dangerous to wait. In my experience around 94% of people with back and leg pain get better on their own without any additional treatment. However, they get better not over hours or days but weeks. Eighty four percent get better after six weeks, and the full 94% improve over 12 weeks (about 3 months).
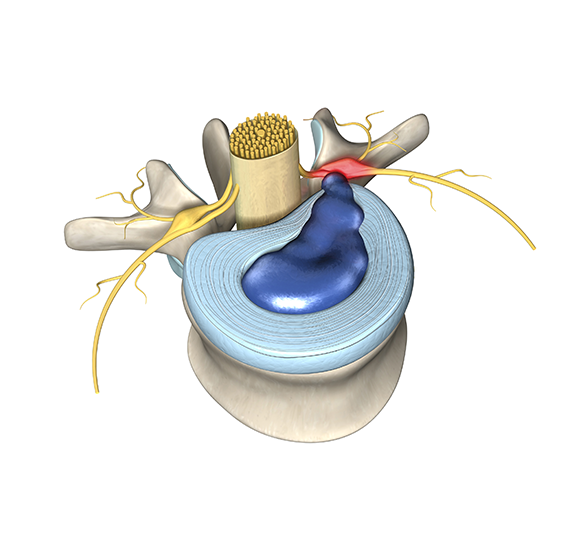
In order to make good decisions about your own body, you need to understand what it means to have a disc herniation, and how your body deals with it.
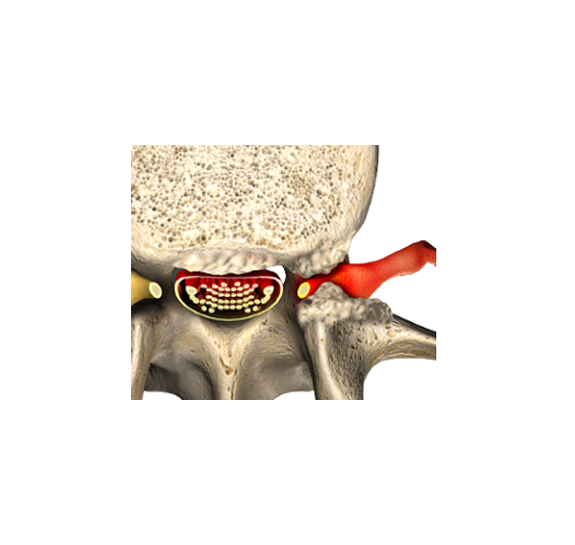
One of the peculiar things about the discs in your lower back is that they do not have their own blood supply. It is through the blood supply that your body recognizes what is part of ‘you’ and what is not. When a disc “herniates” the soft, inner part goes through a rip in the tough outer part. Pat’s body did not “know” that the soft inner part is part of him. So, his body generated an inflammatory response.
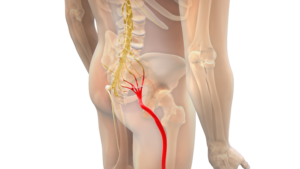
The weird part is that it is the healing that hurts. On the show Pat talked about feeling a “sharp pain” that “went right down my leg.” As his body tried to heal the disc herniation the inflammation spilled over and irritated the neighboring nerve root. That irritation of the nerve root causes the sense of pain going down the leg that people often call sciatica. It also caused a sense of numbness in his leg.

When a herniated disc is the problem the most common solution is to let the body heal itself. But there is a catch. Two of them, actually.
First, the inflammation that reabsorbs the herniated disc is damaging the nerve root. If the healing takes too long, that damage can cause permanent nerve damage. To avoid permanent nerve root damage microdiscectomy surgery to remove the herniated disc fragment is necessary when the disc is causing:
- Weakness that is functionally disabling
- Numbness that is functionally disabling
- Uncontrollable pain
Second, sometimes pain fibers grow into the scar that heals the annulus, and causes permanent low back pain to form the torn disc. This is called discogenic pain.
Learn more about a Herniated Disc.
Is a herniated disc serious?
Herniated discs are extremely common, and most are not serious in the sense that they get better on their own and do not cause permanent problems; however, some can be serious in two ways.
A herniated disc is serious when it causes problems with the neighboring nerve roots due to inflammation or direct pressure. Giant herniated discs, like Pat had, can cause damage to nerve roots making you paralyzed and unable to control your own urine:
If you experience severe weakness, numbness, or incontinence with back pain you may have a giant herniated disc that requires surgery on an emergency basis. If you have severe numbness, weakness, uncontrollable pain, or cannot pee with back pain then go to the nearest hospital that has a neurosurgeon on call. If a hospital is a trauma center, then there is a neurosurgeon on call there.
Second, a herniated disc can happen in conjunction with another serious problem. Infection, tumors, and fractures can all be associated with disc herniation. Fortunately, these conditions are rare, and all of them are easily seen on an MRI (Magnetic Resonance Imaging) scan of your back.
Pat has a history of blood cancer, but it is not the kind of thing that causes tumors that could involve the bones or discs of the spine. When we talked to him Pat also denied having fever, shakes or chills, which makes infection not likely. If you think you have a herniated disc, but you do not have functional weakness, numbness, urinary retention, history of cancer, fever, or recent trauma, then the next step depends on the severity of your pain and the pattern of recovery.
Pat had been to the clinic before, so he contacted us. If you have a lot of pain despite moist heat, rest, and anti-inflammatory medications, or you are not getting better, then see your doctor right away.
What does it feel like to have a herniated disc?
You should think of a herniated disc when the main pain is running down the back and leg and is also causing numbness or weakness in part of the leg. Pat’s history of back pain, leg pain, numbness and weakness are typical of what people feel when they have a herniated disc. The details depend on what the disc. If the disc causes compression of a nerve root, then you may feel pain, weakness, or numbness in the part of your body served by that nerve root.
Pat described a “sharp” pain going down his left leg. This is usually due to inflammation your body generates to try and heal the herniated disc. He also noted numbness in the left leg. Pat’s disc was so large that it affected more than one nerve root; he had numbness in the groin, thigh, and calf.
What is the best treatment for a herniated disc?
Most people with a herniated disc will get better on their own without the need for further treatment over days to weeks. Pat had a history with the clinic, so he came to see us. But for most people the best treatment for pain from a herniated disc depends on how long you have had it.
First Six Weeks
We advised Pat to try rest, moist heat, and anti-inflammatory drugs. Rest means light activity. Tylenol is the safest anti-inflammatory drug. If Tylenol is not enough, you can try ibuprofen (2 tablets every 8 hours with food) or Alleve (one tablet every 12 hours) and Prilosec (one tablet a day). Prilosec is to prevent an ulcer caused by acid due to Alleve or ibuprofen. You can consider acupuncture or chiropractic treatment. Braces and exercise do not work well in this phase. Narcotics and muscle relaxants should be avoided.
Pat did not have any red flags. If he did, he would need to see a surgeon on an emergency basis, the same day.
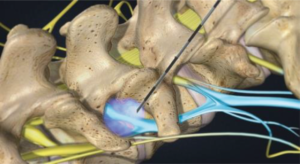
Although not severe, Pat’s leg pain was associated with numbness or weakness, so he got an MRI right away; most of the time an MRI is not needed in the first six weeks. Pat’s MRI showed a giant herniated disc. For herniated discs causing severe pain without numbness or weakness epidural injection is an option. Epidural injection relieves pain temporarily, buying you time for the body to heal. In Pat’s case, he skipped the epidural injection because he had so much hip weakness that if he was left in that position his gait would be permanently altered.
After 6 Weeks
Pat was referred to surgery because he had a giant disc herniation and motor weakness. Physical therapy may be considered in this phase. If 12 weeks (about 3 months) have gone by and someone still has the pain is something structural. Hang in there.
Many patients with herniated discs will choose epidural injection in this phase of recovery. Your doctor will get an x-ray of your back and refer you to physical therapy if appropriate. If you fail to improve over three weeks and there is a lot of leg pain, then your doctor will send you for an MRI of your lower back. If the MRI shows a herniated disc as the cause of your pain, then they may refer you to a pain management doctor for epidural steroid injection.
During the injection, a needle is placed under x-ray guidance outside your spine and a cocktail of steroid and numbing medicine administered.
Learn more about Epidural Injection – Phoenix Spine & Joint (bestpracticehealth.com)
No matter what, if you are not improved after 12 weeks (about 3 months), then your doctor will refer you to an orthopedic spine or neurosurgeon as appropriate.
After 12 weeks (about 3 months)
If you are still having trouble 12 weeks (about 3 months) after the pain started, then it is time to have an MRI if one was not done already and see a surgeon. They will advise you on any structural problem that may be treated in your back to relieve your pain. The use of microdiscectomy surgery was established by the surgeon experience, case series, and eventually a randomized controlled trial – the NIH sponsored SPORT (Spine Patient Outcomes Research Trial). Microdiscectomy surgery is considered the standard of care by professional societies and is covered by Medicare as well as all commercial health insurance for the treatment of MRI-confirmed lumbar disc herniation with motor or sensory deficit as well as uncontrolled pain after the failure of appropriate conservative care.
Learn more about Microdiscectomy.
- Post Tags:
- Pg - Microdiscectomy
- Posted In:
- Herniated Disc With Sciatica