Oxy and Vicodin pretend to be cures, but they are a mask that makes pain worse
Oxy and Vicodin pretend to be cures, but they are a mask that makes pain worse https://bestpracticehealth.com/wp-content/uploads/2023/06/Oxy.png 1024 535 Best Practice Health Best Practice Health https://bestpracticehealth.com/wp-content/uploads/2023/06/Oxy.pngBy Grace Lieberman
Chronic pain is overwhelming and debilitating, so patients tend to understandably trust their doctors implicitly and are hesitant to change a system that provides relief, however small. The reality is, though, that opioids do not effectively treat chronic pain. In many cases they even increase pain and create new health issues.
It is easy to feel like there is no other choice than heavy drugs, but there are options out there for long term pain solutions that do not cause more problems.
Pain mismanagement and choosing a new path
Donna Whitfield is a retiree from Central Florida. She returned to her hometown from Pensacola to help care for her mother and brother after retiring early due to multiple health issues.
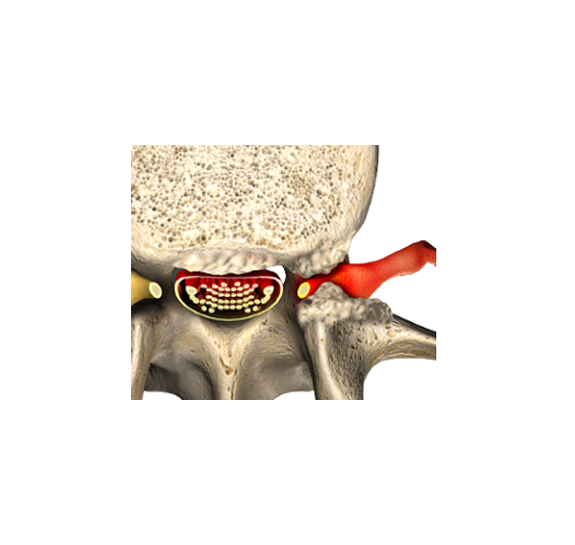
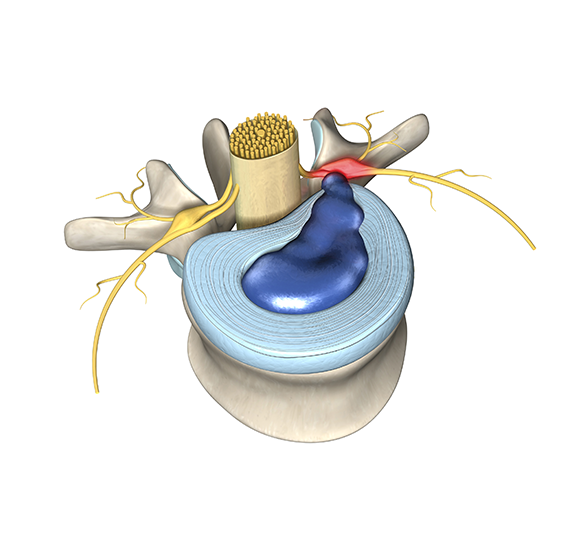
Donna has struggled with fibromyalgia and diabetes in the past. For decades she has also been dealing with constant waves of back pain from spinal stenosis. Recently, the pain has been worsening and spreading to her hips, legs, and feet.
“I hurt all the time. It is just different degrees, you know, sometimes it is worse than others,” Donna said.
After her existing conditions, a back injury, and a broken hip, Donna chalked up her pain to a combination of her medical history and age.
“But then it progressively got worse, and now it’s both legs and it’s further down,” Donna said. “It’s just constant, and I stumble around, and my legs give away.”
Donna has been working with pain management doctors for decades, but she still struggles with pain daily. For years she has been prescribed a combination of narcotic pain medications that she cannot even take as often as directed because they cause her to feel disoriented.
After her doctor retired a few years ago, Donna bounced around to different physicians. Eventually, Donna was able to get MRI (Magnetic Resonance Imaging) imaging that showed severe spinal stenosis. She was finally recommended to see a surgeon.
Spinal stenosis cannot be treated with medications. Instead of getting the treatment she needed, the narcotics simply covered up her symptoms, masking the real problem. The scary part is that Donna could have died: failure to treat spinal stenosis long term leads to paralysis, urinary tract infection, and eventually death.
The truth about opioids and chronic pain
It is common knowledge that cases of opioid addiction and overdoses have skyrocketed in recent years.
According to the Centers for Disease Control and Prevention, drug overdose deaths in the U.S. have quintupled since 1999. The National Institutes of Health reports that over 106,000 people died from drug-involved overdose in 2021, including both illicit drugs and prescription opioids.
In the past, doctors have prescribed opioids for managing pain. This is often done out of care for the patient with the goal of making sure their pain is minimized as much as possible. Some, however, prescribe medications recklessly while prioritizing profit over their patients’ wellbeing.
One might think that reduced pain automatically means positive results, but opiate therapy simply covers up pain and prevents you from addressing the source.
In Donna’s case, doctors knew she had spinal stenosis. But instead of offering real, long-term solutions, they kept prescribing opiates and other treatments that are proven ineffective for stenosis.
Watch the whole interview here:
When it’s time to fire a drug pushing doctor and get the treatment you need | Spinal stenosis
In recent years, there have been hundreds of indictments related to doctors fraudulently distributing opioids and pharmaceutical companies bribing physicians to promote their product. Efforts are being made to crack down on predatory practices in medicine, but addiction is still a major risk and can affect anyone.
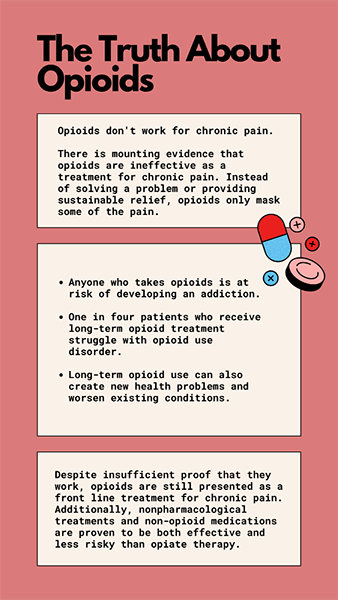
Opioids have important uses in medical treatment for acute pain and temporary relief in emergency scenarios and to control pain due to cancer in the terminally ill. But despite commonly being prescribed for chronic non-cancer-related pain, research proves this is only a temporary solution and is damaging to the patient’s long-term health.
The diminished efficacy of opioids in long term treatment is looked at as the patient “building up a tolerance” to the drug. But what that really shows is the ineffectiveness of the drug for long term treatment.
Instead of framing the problem as the drug’s failure to serve the patient, the idea of building a tolerance to the drug makes the patient’s body responsible for not accepting the right treatment. The body’s response to treatment should determine its effectiveness. So, when a treatment only proves to be effective for a short time, that is a problem with the treatment, not the dosage or the patient.
Think about trying to repel mosquitos in the summer. If you put out a bug repellant and it worked for one day, but then bugs came swarming again, the solution would be to try a new way of repelling the bugs, not adding more of the same thing. Moreover, if you kill the bugs but neglect a bucket of still water where they are laying eggs nearby, they will just keep coming back.
Addiction from prescribed opioids sneaks up on people, and it is hard to see that there is a problem until it is too late. Getting treatment can also be difficult if you feel like the drugs are keeping you from falling back into immense pain.
The reality is that opioids do not help chronic pain. At best, they mask certain pain while causing new sources of it with their damaging side effects.
Substance use disorder and overdose death are the prominent dangers of opioid use, but they are not the only ones. Some risks of long-term opioid use include bone fractures, heart attack, sleep apnea, immunosuppression, constipation, bowel obstruction, and tooth decay from dry mouth. Opioid use can also cause hyperalgesia, an increased sensitivity and response to pain, worsening the very problems the drug was intended to treat.
Managing pain another way
Whether it be well meaning ignorance or predatory practices, doctors have historically prescribed pain medication incorrectly at a large scale. In Donna’s case, despite years of poor results, she was continuously prescribed potentially damaging drugs.
People suffering with chronic pain can feel trapped into taking dangerous medication while looking for any relief. But innovations in medical care and a shift in the culture of medicine has started to combat that.
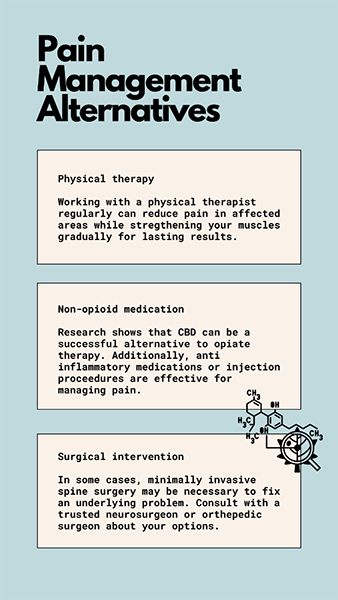
Donna became fed up with the treatment from her previous doctors and started seeking new care. She tries to rely more on medical marijuana and CBD for pain relief and was also recommended for minimally invasive spine surgery and physical therapies.
Back pain and its causes vary significantly across individuals and finding effective treatment requires a personalized approach.

There are more medications than just opioids to treat pain. Some doctors recommend certain nonsteroidal anti-inflammatory drugs or psychiatric medications. Research on CBD’s benefits and drawbacks is still relatively new, but the consensus is that it is a great alternative to opioids for chronic pain management. Although non-addictive, each pharmacological therapy comes with its own set of risks and side-effects. Patients should always work closely with their physician to find the right medications for them.
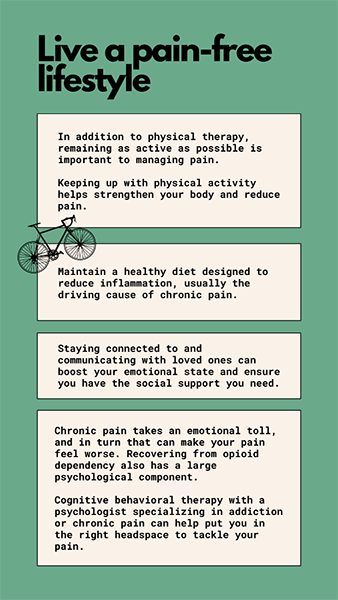
Physical therapy and other forms of movement therapy such as Tai Chi and osteopathic manipulative treatment are also rising in popularity. In severe cases, consulting with a surgeon about minimally invasive spine surgery may be recommended.
Finding what is best for you
Living with pain, and attempting to manage it, can feel like an impossible task. The overwhelming nature of pain can cause complacency with ineffective treatment or put a patient off from seeking care altogether.
No matter how it seems, there’s options to get off harmful drugs and treat addiction while also seeking real, lasting pain treatment.
One key factor in switching to a new form of pain management is finding a doctor committed to taking you off the medications you wish to stop and not prescribing more. Most opioid users can safely reduce their dose by one pill every three days until they are off the medication.
For those recovering from dependency or addiction to opioids, your doctor may recommend cognitive behavioral therapy (CBT) with a psychologist specializing in addiction.
Although finding trusted providers and the right treatment for you can take time and effort, it is worth it to find a solution for your pain that does not cause more problems.
- Posted In:
- Addiction